PIOA Supervision Mission in Rabaul, East New Britain Province, Papua New Guinea (PNG) April 2018
Dr. med. Philipp F. Stillhard, General- and Trauma Surgeon, incl. Orthopaedic Trauma
Rabaul
Rabaul is a town in the East New Britain Province, on the Island of New Britain. Until the huge volcanic eruption in 1994, Rabaul was the province capital. During the eruption, a rain of ash destroyed 80% of the buildings. Rabaul’s history is exciting. Before World War I, the city was under German New Guinea administration followed by The British Empire and later on became the capital of the Australian mandated Territory of New Guinea. During World War II, Rabaul was captured by the Japanese and in 1942 it became the main base of Japanese military in the South Pacific. Military installations from this time can still be seen. After the Second World War, the area returned to Australian administration until independence in 1975 (modified from Wikipedia)
The Nonga General Hospital is the main hospital in East New Britain Province and is responsible for over 350’000 people in the area, some patients even come by boat from New Ireland Province. The hospital was recently renovated, and the wards and OT are in quite a good condition. Next to several departments, such as surgery, internal medicine, radiology, accident and emergency, gynaecology, laboratory and so on, there is an ICU as well as an Intermediate Care.
My accommodation is a simple hotel, called Rabaul Hotel only 10 minutes from the Hospital by car. The daily transfer is organized from the hospital.

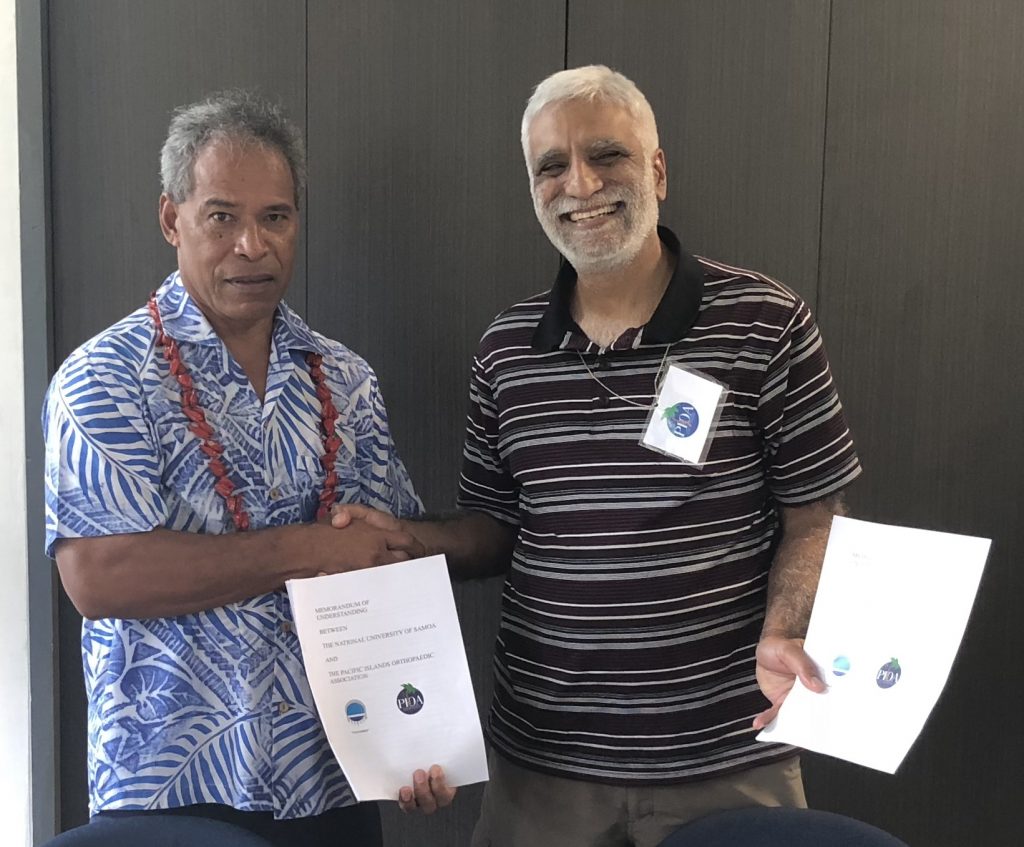
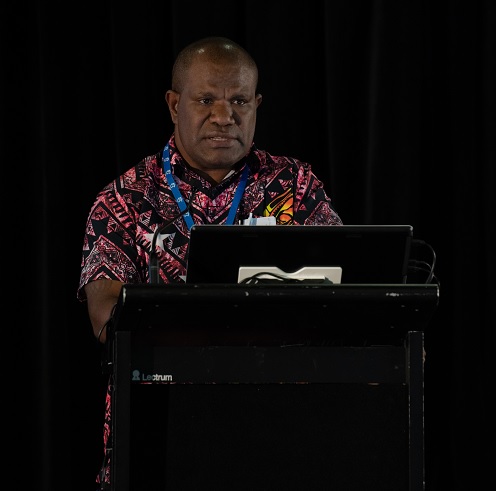
The Head of Surgery and PIOA trainee Dr. Kevin Lapu, is a highly experienced surgeon with a brilliant surgical hand and huge empathy, he is working in a team of six, one consultant, 2 registrars, 2 residents and himself. The buildings have been recently renovated and look nice. On closer examination, you realize that certain things are not working properly. The surgical ward is divided in three rooms: the first room accommodates general surgical patients, the second, orthopaedic trauma patients and the third, infected and diabetic surgical problems. Energy and water supply seems sufficient, and they have their own generator available for emergency reasons. Right now, 2 ORs are running with a sterilisation and packing unit. A minor theatre was recently renovated and will open soon for wound debridement. One consultant and clinical nurses provide an anaesthetic service, which is working more or less efficiently. Basic instruments and reduction clamps are available as well as a recently ordered power-drill, unfortunately they are without a quick coupling and oscillating saw. A full small and large fragment set with screw rack, wire and external fixator set are available. Basic procedures such as external fixations, pin tractions and uncomplicated small and large fragment cases can be done safely. For more complex cases the team needs more training. Unfortunately, there is no intraoperative imaging available right now.
The OT team is working very thoroughly but without a lot of experience in orthopaedic trauma surgery. The topic, aseptic workplace should be discussed with infectiologists. The management of plates and screws stock should be taught by an experienced OT-nurse. Finally, I went on to count all plates and screws and wrote it down in an Excel file, which I kindly received from Dr. Alois Mouemuem under the note: “helping PIOA trainees is caring for them”.
My first day at Nonga General Hospital, a Sunday, we did an extensive ward-round, discussed all the orthopaedic cases for its non-operative or operative treatment. We have reviewed patients from the surgical ward and from the out-patient clinic, especially with non-unions and mal- unions around the upper extremity and some cases of infected osteosynthesis and acute and chronic osteomyelitis.
During my first days, I met everybody important from the administration, the medical officer, supervisor and CEO included.
The following are just some cases we discussed and operated on together during my stay in Rabaul:
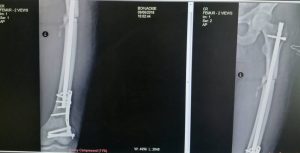
A 40 year old man with a history of left femur fracture. ORIF was done with a K-Nail and cerclage wires more than a year ago and got infected. The clinical examination shows a 20° externally rotated left leg with a sinus around the old approach with some pus and a gluteal decubital ulcer. Actual XRay findings: osteolytic lesion around the nail and an avital fragment, clearly a postoperative infection. The reason for the decubitus is identified, the nail juts out of the greater trochanter, much more than it should.

After discussing the problems of rotational instability using K-Nails without locking bolts, the management of infected osteosynthesis and the problem nails sticking out of the greater trochanter, we planned a revision surgery for the patient. First of all, we excised the decubital ulcer and removed the nail from there. Secondly, we excised the old scar with its sinus. After removing the cerclage wires, we tested the bone fragments with the “Cocker Test”, removed all necrotic bone, applied pins to the distal fragment in 20° external rotation and to the proximal fragment straight laterally. Finally, we rotated the distal fragment by 20° and applied an unilateral external fixator.
Another case was a lady presenting with a humeral shaft fracture treated with a POP over 4 weeks. The clinical examination and the x-ray XRay findings motivated us to proceed with ORIF.

From the teaching aspect, there are different goals to mention. To begin with, there is the topic “different approaches to the humerus”. After discussing the benefits and drawbacks of the different approaches, we have decided to go for an anterolateral approach which was never done before by Dr. Kevin Lapu. The second point was the issue “AO-principles” and how can we get compression to a transverse fracture.
The last case to mention was a lady in her thirties who presented with a displaced R forearm fracture. Initially the fracture was treated conservatively during 4 weeks. The indication for ORIF was to correct the displacement by anatomical reduction and therefore avoid a poor functional outcome.

We chose the Thompson approach to the radius and a straight approach to the ulna, removed the callus, achieved anatomical reduction. The radius was fixed by a 7-hole DCP and the ulna by 6-hole 1/3 tubular plate.
Next to all the operations and teaching in the OT, we discussed fracture management for open fractures, paediatric fractures and fractures around the humerus. Another, non-surgicaI topic, I tried to cover, was the use of hand disinfectant and gloves during the ward round and change of dressings. Furthermore, I got the chance to talk about the idea behind PIOA and general aspects in paediatric fracture management during a grand-round meeting with some members of the hospital medical board. Hopefully, they got my message about supporting Dr Kevin Lapu for his PIOA training as well as financial support for further instruments and implants for operative fracture management.
Early Sunday morning, we walked up to the top of the volcano. Just amazing and I am grateful for this hike.

Future ideas:For sure, more supervision missions should be organised for the Nonga General Hospital. Furthermore, a C-arm would be helpful as well as an oscillating saw.
The hospital should keep going on with buying some implants and screws. The shorter sizes of screws in the small fragment set have already run out. Also, some small reduction clamps (pointed forceps (2x) and crab-claw clamp (1x), new external fixator bars and Schanz screws should be organized. There is also a need to teach ORP about use and maintenance of orthopaedic equipment, as well as stock-keeping and ordering replacements in time.
“…the ward is our library, patients our books we are learning from…”
Dr. Kevin Lapu
Philipp F. Stillhard, April 2018







 The 2018 visits were again supported financially by the SST. Travel expenses, especially the flights to, from and within PNG, are a substantial part of the project costs. Living costs in PNG are as well astounding, if the Hospitals don’t provide accommodation for foreign doctors. This is especially true in the Highlands, where accommodation costs even for very basic rooms exceed 100 USD per person per night by far.
The 2018 visits were again supported financially by the SST. Travel expenses, especially the flights to, from and within PNG, are a substantial part of the project costs. Living costs in PNG are as well astounding, if the Hospitals don’t provide accommodation for foreign doctors. This is especially true in the Highlands, where accommodation costs even for very basic rooms exceed 100 USD per person per night by far.